Diabetic Retinopathy
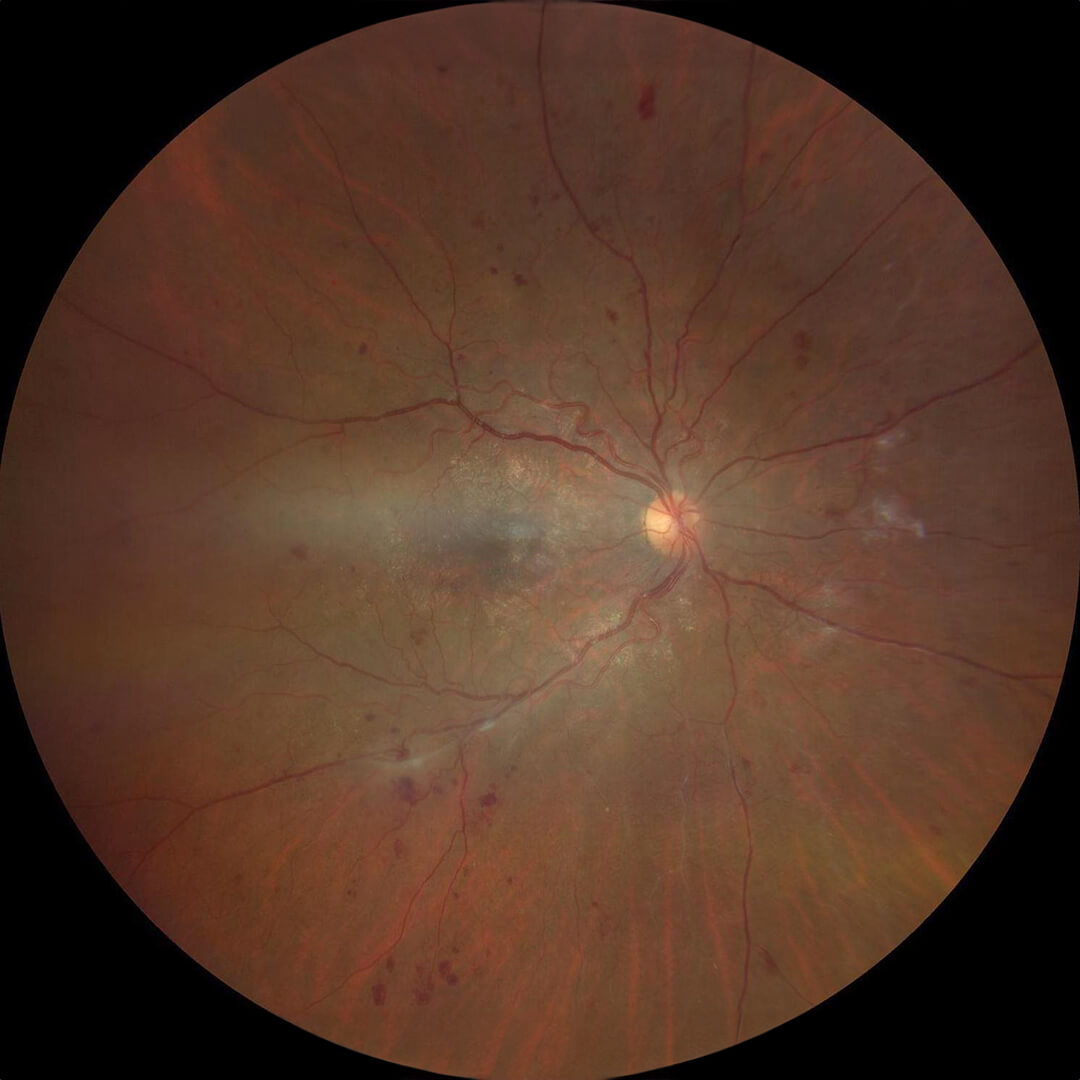
Scattered retinal hemorrhages due to diabetic retinopathy.
Diabetes is a disease that has multiple effects throughout the body. The most serious eye problem is diabetic retinopathy, where the blood vessels in the retina are affected. This damage builds slowly over many years.
When to See a Diabetic Eye Specialist
It is recommended that patients with type 1 diabetes receive their first exam 5 years after the diagnosis of diabetes, but type 2 diabetics should get an exam shortly after diagnosis. Type 2 diabetics often have diabetes silently for many years before diagnosis, so they can have significant retinal damage even at the time of diagnosis. The damage to the blood vessels is irreversible, but the process can be slowed down dramatically with good control of blood sugars as well as other factors such as blood pressure and cholesterol.
Stages of Diabetic Retinopathy
Diabetic retinopathy in the earliest phase is invisible on examination (the “diabetes without retinopathy” phase).
The middle phase of diabetic retinopathy is nonproliferative (background) diabetic retinopathy. This involves scattered hemorrhages throughout the retina that don’t generally cause vision loss without other complications. This stage does not require any treatment other than blood sugar control, although it becomes increasingly important that the retina is monitored for signs of complications such as proliferative diabetic retinopathy and diabetic macular edema. The complications of diabetic retinopathy are best treated if caught early, so regular follow-ups are very important.

Bleeding from diabetic retinopathy obscures the retina.
The next stage of diabetic retinopathy is the transition to proliferative diabetic retinopathy. Here, abnormal blood vessels (neovascularization) grow from the retina into the vitreous gel that fills the middle part of the eye. With smaller abnormal vessels, there are no symptoms. In many cases, relatively prompt treatment of proliferative disease is needed.
Possible Complications
There are complications of abnormal blood vessels that cause vision loss and even blindness with increasing frequency as the vessels grow larger.
Vitreous hemorrhage is the most common complication, where the abnormal blood vessels break and bleed into the vitreous gel. The sudden onset of floaters is often the first symptom, but the vision loss can be severe. The hemorrhage can clear spontaneously after the abnormal blood vessels are treated with injections or laser, but sometimes vitrectomy surgery is needed to clear away the blood.
Traction retinal detachment is a less common complication where the abnormal blood vessels contract and pull the retina out of place. If off center and stable, it does not need to be treated directly. However, vitrectomy surgery is needed to relieve the traction and allow the retina to settle down for traction retinal detachments that involve vision loss.
Another complication seen both with proliferative and non-proliferative diabetic retinopathy is diabetic macular edema, where damaged blood vessels in the retina slowly leak fluid leading to retinal swelling. If the swelling is away from the center, it does not affect vision. However, if the swelling affects the central macula (the center of the retina where sharp central vision is located), it can lead to considerable blurriness although not blindness. Although somewhat less urgent than proliferative disease, treatment often results in stabilization and possibly some improvement.
Diabetic Retinopathy Treatment
The first treatment available was panretinal laser treatment, where laser treatment is placed in a scatter fashion throughout the side area of the retina. This treatment is often done in a couple of sessions. There is some (mostly tolerable) pain during the procedure.
The mainstay of treatment is intravitreal injection of medication, primarily anti-VEGF agents. These drugs stabilize leaky vessels and can reduce swelling (edema), although some edema is resistant to treatment. These are easier to tolerate with less peripheral vision changes, but they need to be done on an ongoing basis to keep the blood vessels at bay. Light laser treatment to seal leaky areas is in many cases a supplemental treatment, but sometimes laser is done primarily. Vitrectomy surgery is done as a last resort unless there is abnormal tissue causing the swelling that needs to be removed.
